Understanding whether Medicaid covers braces in Colorado can be confusing. This article aims to clarify the coverage details for orthodontic treatment under Colorado’s Medicaid program, known as Health First Colorado. We’ll explore eligibility requirements, coverage limitations, and the application process, helping you navigate the path to a healthier smile.
Understanding Medicaid Coverage for Braces in Colorado
Health First Colorado offers orthodontic benefits, including braces, for children and young adults who meet specific criteria. The coverage isn’t automatic and depends on demonstrating medical necessity, not just cosmetic improvement. This means the misalignment must significantly impact oral health and function. Coverage is typically limited to individuals under 21.
Does Colorado Medicaid cover dental? Yes, and that includes orthodontic care in certain circumstances. The program prioritizes treatment for conditions like severe malocclusions that affect chewing, speaking, or breathing. While purely cosmetic concerns are generally not covered, the line between medical necessity and cosmetic improvement can sometimes be blurred, requiring a thorough evaluation by a qualified orthodontist.
does colorado medicaid cover dental
Who is Eligible for Medicaid Braces in Colorado?
Eligibility for Medicaid braces in Colorado primarily hinges on age and medical necessity. Generally, individuals under 21 enrolled in Health First Colorado are eligible for consideration. A qualified orthodontist must determine if the malocclusion is severe enough to warrant treatment. Documentation, including X-rays and dental models, is usually required to support the claim. Income guidelines for Health First Colorado also apply.
Qualifying Medical Conditions for Braces Under Medicaid
Several conditions can qualify an individual for Medicaid-covered braces. These include severe overbites, underbites, crossbites, and open bites, as well as overcrowding and spacing issues that impact oral function. Cleft lip and palate are also often covered. Each case is evaluated individually.
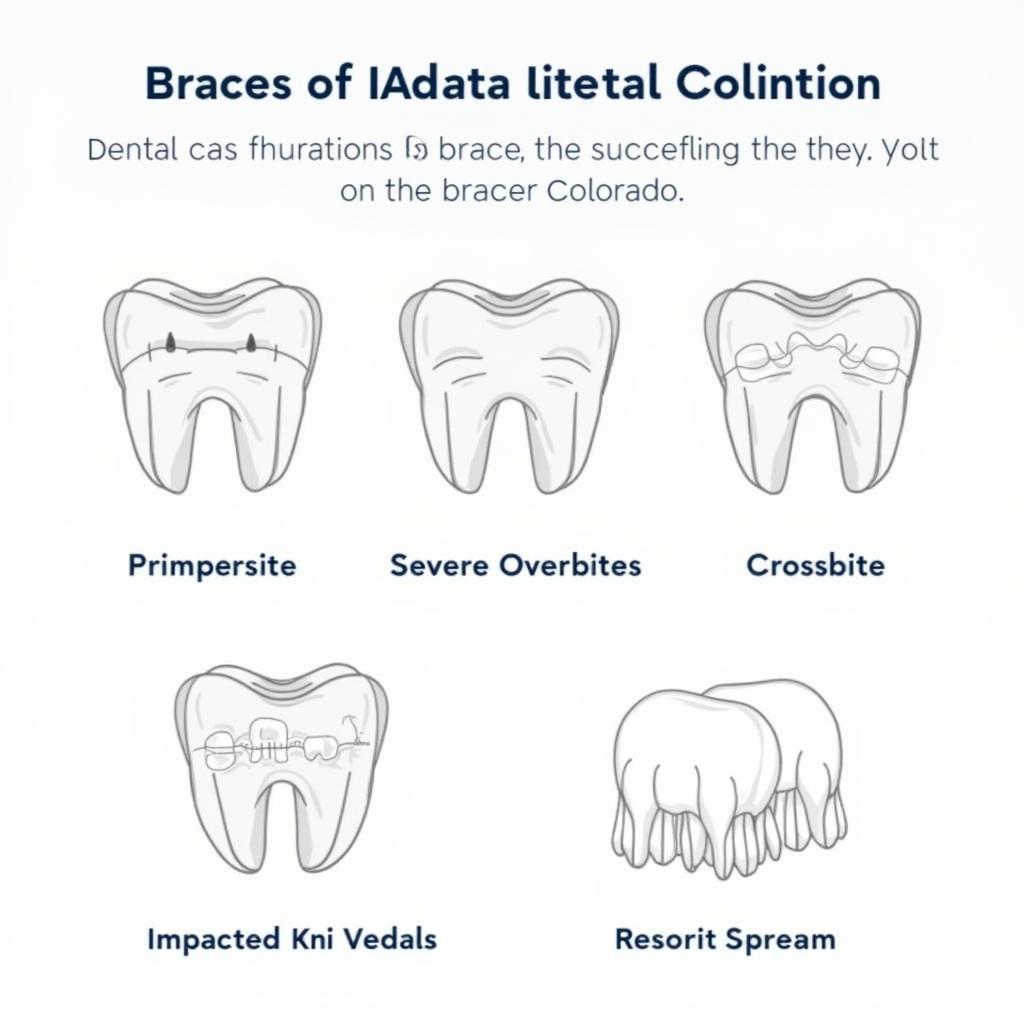 Qualifying Conditions for Medicaid Braces Coverage
Qualifying Conditions for Medicaid Braces Coverage
How to Apply for Medicaid Braces in Colorado
The application process for Medicaid braces typically involves several steps. First, ensure you’re enrolled in Health First Colorado. Then, find a participating Medicaid orthodontist. The orthodontist will conduct a comprehensive evaluation and submit a prior authorization request to Health First Colorado if braces are deemed medically necessary. Approval can take several weeks.
What does Medicaid cover for dental for adults in Colorado? While orthodontic coverage is typically for those under 21, adults can still access other essential dental services through Health First Colorado. Knowing what is and isn’t covered can help you plan your dental care effectively.
what does medicaid cover for dental for adults in colorado
How Much Does Medicaid Cover for Dental in Colorado, Specifically Braces?
The amount Medicaid covers for braces in Colorado varies depending on the individual’s treatment plan. Generally, Health First Colorado covers a significant portion, if not all, of the medically necessary orthodontic treatment. It’s crucial to discuss the specifics with your chosen orthodontist and Health First Colorado to understand any potential out-of-pocket costs.
how much does medicaid cover for dental in colorado
Conclusion
Navigating Medicaid coverage for braces in Colorado requires understanding the eligibility requirements and application process. By focusing on the medical necessity of treatment and working closely with a participating orthodontist, you can improve your chances of securing coverage for necessary orthodontic care. Remember, a healthy smile contributes significantly to overall well-being.
FAQ
- Does Medicaid cover braces for adults in Colorado? Generally, orthodontic coverage is limited to individuals under 21.
- Can I choose any orthodontist for Medicaid braces? You must select an orthodontist who participates in the Health First Colorado program.
- What if my application for Medicaid braces is denied? You have the right to appeal the decision.
- How long does treatment with braces typically last? Treatment time varies, but it usually lasts between 18 and 36 months.
- Will Medicaid cover retainers after braces are removed? Yes, retainers are typically covered as part of the overall orthodontic treatment.
- What are the age limits for Medicaid braces coverage in Colorado? Coverage usually extends to individuals under the age of 21.
- Can I get Invisalign through Medicaid in Colorado? Coverage for Invisalign depends on medical necessity and may not always be approved.
Dr. Emily Carter, a Denver-based orthodontist specializing in Medicaid cases, emphasizes that “early intervention is key for successful orthodontic treatment, particularly for children. Medicaid coverage allows many children to access necessary care that would otherwise be unaffordable.”
Dr. David Ramirez, a pediatric dentist with over 20 years of experience, adds, “Parents should be proactive about their children’s dental health. Regular checkups and early diagnosis of malocclusions can significantly improve treatment outcomes and leverage Medicaid benefits effectively.”
For further assistance, please contact us at Phone Number: 0373298888, Email: [email protected], or visit our office at 86 Cau Giay, Hanoi. Our customer service team is available 24/7.

